As a woman, you have unique health needs. One of the most important things you can do for your health is to be familiar with your body and know how to recognize any changes, especially when it comes to breast health. By performing a monthly breast self-exam, you can get to know the look and feel of your breasts and quickly identify lumps or other changes that may be potential signs of breast cancer.
Breast self-exams can be a helpful tool in understanding your breast health and how your breasts change over time. By making this a regular part of your monthly health routine, you can become familiar with your breasts and maintain good breast health practices in between routine screening mammograms.
Breast Self-Exams: Importance and Limitations
While the recommended age for women to start annual screening mammograms is 40, you can begin doing self-exams as early as in your twenties and in addition to clinical breast exams by your physician during your annual well visit. Routine self-exams help you to become more “breast aware” and familiar with the look and feel of your breasts, so you can better determine what may be normal for you or what may require further attention from your physician.
If you detect anything out of the ordinary during a self-exam, such as a breast lump that was not there previously, you should discuss your concerns with your doctor right away. Your doctor can provide a clinical breast exam and better determine the need for follow up, such as breast imaging, so that a diagnosis can be made. While breast self-exams are important, there are also limitations, which can include the following:
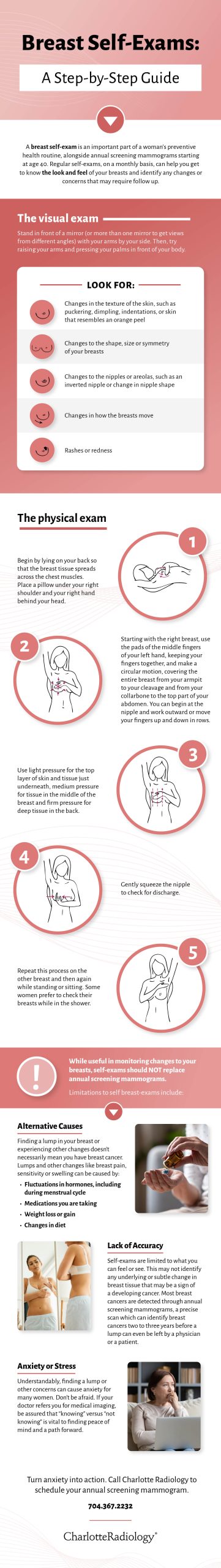
- Alternative causes: Finding a lump in your breast or experiencing other changes doesn’t necessarily mean you have breast cancer. Lumps and other changes like breast pain, sensitivity or swelling can be caused naturally by fluctuations in hormones occurring monthly for women, especially around their menstrual cycle. Changes in your breasts can also be caused by other factors, like weight gain or loss, medications you are taking, changes in diet, or other variables.
- Lack of accuracy: Self-exams are limited to what you can feel or see versus any underlying or more subtle change in breast tissue that may be a sign of a developing cancer. In fact, most breast cancers are detected through annual screening mammography — advanced imaging technology that can identify breast cancers two to three years before a lump can even be felt by a physician or patient. Early detection is key to diagnosing and treating breast cancers in their earliest stages.
- Anxiety and stress: Understandably, finding a lump or other concern can cause anxiety for many women. Don’t be afraid. It’s important to turn anxiety into action and discuss your concerns with your physician to determine next steps. If your doctor refers you for medical imaging, be assured that “knowing” versus “not knowing” is vital to finding peace of mind and a path forward, regardless of whether breast cancer is present — or more likely — not present.
For these reasons, self-exams should not be done in place of annual screening mammograms.
Follow your doctor’s recommendations for screening and be sure to notify your doctor if you find anything unusual in a self-exam or if you experience any symptoms.
Read More: 8 Common Breast Cancer Myths Debunked
What You Need to Know Before Doing a Breast Self-Exam
Before doing a breast self-exam, it’s a good idea to ask your doctor for a demonstration to learn the proper method. This can help ensure you are getting the most benefit from your self-exams.
It’s also important to know the best time to perform a self-exam every month. Because your menstrual cycle can impact the feel and tenderness of your breasts, experts recommend performing a self-exam about five to ten days after the start of your period.
How to Visually Inspect Your Breasts
The first part of a breast self-exam involves checking for changes in the appearance of your breasts. Stand in front of a mirror (or more than one mirror to get views from different angles) with arms by your side and look for:
- Changes in the texture of the skin, such as puckering, dimpling, indentations, or skin that resembles an orange peel
- Changes to the nipples or areolas, such as an inverted nipple or change in nipple shape
- Changes to the shape, size or symmetry of your breasts
- Rashes or redness
Next, do the same with your arms raised and with palms pressed in front of the body. Be aware of the way the breasts move.
How to Perform a Physical Breast Self-Exam
To perform the physical exam:
- Begin by lying on your back so that the breast tissue spreads across the chest muscles. Place a pillow under your right shoulder and your right hand behind your head.
- Starting with the right breast, use the pads of the middle fingers of your left hand, keeping your fingers together, and make a circular motion, covering the entire breast from your armpit to your cleavage and from your collarbone to the top part of your abdomen. You can begin at the nipple and work outward or move your fingers up and down in rows.
- Use light pressure for the top layer of skin and tissue just underneath, medium pressure for tissue in the middle of the breast and firm pressure for deep tissue.
- Gently squeeze the nipple to check for discharge.
- Repeat this process on the other breast and then again while standing or sitting. Some women prefer to check their breasts while in the shower.
Reasons to Contact Your Doctor
If you notice any of the following possible signs of breast cancer, contact your doctor:
- A new lump, which could feel like a hard, painless mass or be soft, round and painful
- Thickening of tissue in the breast or armpit area
- Pain or sensitivity in the breast or nipple or underarm
- Changes to the size or shape of the breast or nipple
- Nipple discharge that is bloody, milky or watery
- Redness, itchiness or warmth in the breast
It’s important to remember breast pain, sensitivity, and lumps can occur naturally with your menstrual cycle, and any changes you find in your breasts don’t necessarily indicate breast cancer. Talk to your primary care provider or OB/GYN, who can determine whether additional testing or imaging is necessary.